The Most Neglected Subgroup: Vaccination in COVID-recovered Children
COVID-19 vaccine EUA for 5-11 year olds is expected, which will be used to construct rigid mandates. The FDA and CDC need to consider the specific risk-benefit of the COVID-recovered child.
As the U.S. COVID-19 vaccination saga continues to unfold, there are two head-scratching controversies that remain at the forefront of the debate. First, does previous SARS-CoV-2 infection confer sufficient immunity to compete with vaccination? This question has been asked since vaccinations began in December, 2020 — and the CDC still refuses to officially acknowledge natural immunity. Second, and more recently, do children as young as 5-11 years of age need to be be vaccinated against COVID-19? The FDA is currently assessing the safety and efficacy of the Pfizer vaccine in this age group, but it is expected they will grant the EUA. The application is here.
The intersection of these two groups— young children <and> the COVID-recovered, represents perhaps the most neglected (but probably large) subgroup also near and dear to our hearts. While numerous studies have independently looked at vaccine safety and efficacy in various age groups (as young as 12-16 years) and natural immunity, no studies exist on the COVID-recovered child. In fact, the Pfizer trials could barely calculate a vaccine efficacy at all for the entire adolescent age group (having to rely on an intermediate technique called “immunobridging”, let alone the specific safety and efficacy on COVID-recovered children. Yet, these COVID-recovered children would be subject to any applied mandate.
The COVID-recovered population in this 5-11yo age group could be extremely large, with 1.8 million documented infections in this age group, and with 1 in 4.2 infections reported, up to 8 million children may have had asymptomatic exposure. What is the expected benefit of vaccination to this group, and is it outweighed by the risks? Any parent with adolescent children, especially COVID-recovered, should be asking this fundamental question. So, we will consider a basic risk-benefit analysis here, based on the available data and extrapolation from adult data points (because it is the best that we can do).
** What is the BENEFIT of vaccination in COVID-recovered young children? **
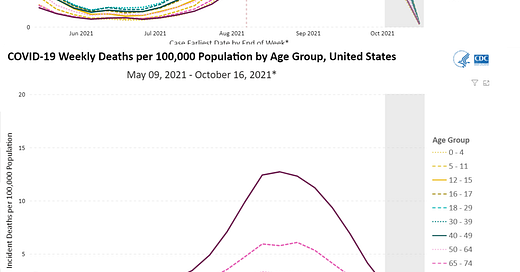
During the earliest phases of the pandemic, children were thought to be relative spared from SARS-CoV-2 infection. However, more recently, the rates infection have been observed to have been increasing — particularly towards the end of summer, and now make up a larger percentage of cases. As of current CDC data, the weekly incidence of infections in 5-11 yos is near peak at 218.3 cases/100k persons, but mortality is virtually unmeasurable at 0.01/100K persons-week. Below is the weekly incidences and mortality, as reported by the CDC.
Hospitalizations in the 5-11 yo age has always been the lowest for all pediatric age groups since the start of the pandemic, at currently at 0.5 hospitalizations /100k persons per week. Cumulatively, there have been roughly 20 hospitalizations/100k over the entire course of the pandemic (Taken from a CDC MMWR publication).
So, to summarize, while unvaccinated 5-11 yos currently have one of the highest rates of infection compared to other vaccinated age groups, the risk of mortality and severe disease still remains the LOWEST amongst age groups. This holds true, despite the fact that this age group is almost exclusively unvaccinated. For our purposes, let us assume that the average rate of infection in 5-11 yos is 1/2 the peak of the most recent wave (~175/100k-week), hospitalizations at its current peak (~0.5/100k-week), and mortality is 0.01/100k-week. Let us attempt to calculate the <absolute> benefit of vaccination for COVID-recovered 5-11 year old children.
These numbers above (per 100k/children 5-11 yo) are for all children, regardless of previous infection history or immune status. While reinfection rates in this 5-11 yo age group have not specifically been studied or published, the protective effect of prior infection in all age groups is considered to be as high as 90% over 8 months, as in this metanalysis, but even more modestly, at 70-80% in the pivotal Pfizer trial.
So, for our purposes in performing a conservative analysis, let us assume that prior infection confers a 75% protective effect in 5-11 yos, as well (for infection, hospitalization, and mortality). The rates of infection, hospitalization, and mortality in the COVID-recovered 5-11 yo (per 100,000 children) are estimated in the table below (fifth column from left).
Therefore, we can expect 5-11 yo COVID-recovered individuals to have a rate of 2275 cases/100k-year, 6.5 hospitalizations/100k-year, and 0.13 deaths/100k-year. The next step is to estimate the incidence rate after vaccination. However, based upon credible adult studies, the vaccine efficacy (VE) for recovered individuals is notably lower than for naive individuals. The Pfizer VE in COVID-recovered individuals was quite low at 6 months, even per their own pivotal trial published in NEJM, in which they found a vaccine efficacy of 19.2% (a Moderna real-world study in Lancet showed and 18-33% VE).
Again, out of being conservative, let us assume that the Pfizer vaccine is 50% effective for COVID-recovered children (this VE is similar to the “famous” KY study and Israel Gazit et. al. study). Then, we would save ~1100 infections, 3.3 hospitalizations, and 0.07 deaths per 100,000 COVID-recovered and vaccinated 5-11yos.
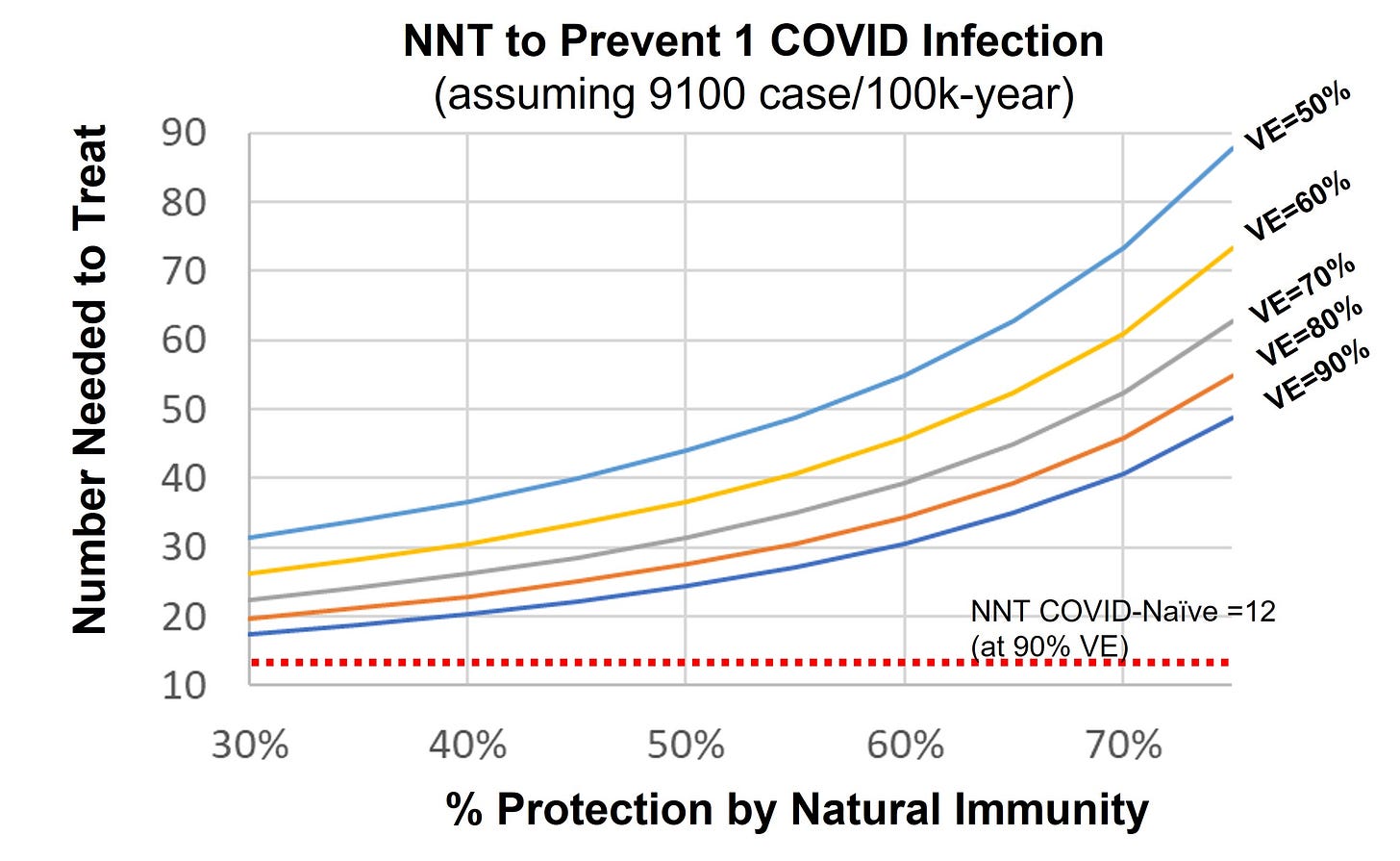
If you have trouble perceiving the size (or lack thereof) of the magnitude of this effect, another way epidemiologists look at this number is the “number needed to treat” or NNT (2nd to last column from right). This number is derived from the reciprocal of the absolute difference in rates — and represents the number of recovered children needed to be vaccinated in order to prevent one case, hospitalization, or death. With these very conservative assumptions, the NNTs are 88, 31k, and 1.5M (2nd to last column)!! For comparison, the NNTs in a similar COVID-naive cohort (assuming 90% VE) would be 12, 4274, and 214k (last column).
In other words, because COVID-recovered children can expect 1/7th of the absolute risk reduction their COVID-naive counterparts would expect, and the baseline risk is small to begin with. And, while the above analysis is based on some basic (conservative) assumptions (% protection of natural immunity, and VE) — below is a basic sensitivity analysis that shows the expected NNT for various levels of immunity protection and vaccine effectiveness. To even begin to consider equivalency of benefit between COVID-recovered and COVID-naive children, you would have to believe that natural immunity offers only < 30% protection and VE in the COVID-recovered >90%. The current data simply does not remotely support this.
Also note, that the above graph is for cases only. Similar sensitivity analysis on hospitalizations and mortality would also show significantly lower absolute impact of vaccination in COVID-recovered children ages 5-11, generally about an order of magnitude less than their COVID-naive counterparts, due to:
Much lower incidences of severe disease in the overall 5-11 yo age group.
A non-trivial (in fact, significant) protective effect from natural immunity (70-90% reduction), as extrapolated from the adult data.
A generally lower vaccine efficacy for COVID-recovered persons, also extrapolated from the adult data.
Therefore, COVID-recovered children ages 5-11 y.o. may be the subgroup that has the least absolute benefit to gain, and should be weighed against the small, but non-zero (and still unknown risks).
** What is the RISK of vaccination in COVID-recovered young children? **
Weighing the benefits of an intervention against the risks it presents is at the nucleus of clinical medicine. Often times, physicians operate in an environment of uncertainty , with imperfect data, and we make intuitive recommendations based on available data, but also individual factors that may modify the calculus. It is not merely good enough to believe that benefit is merely similar to risk, but that benefit greatly exceeds risk. And for a rigid mandate, the benefit must be overwhelmingly greater than the risk.
I do not intend to show here, that vaccine adversity clearly exceeds benefit. In fact, in all likelihood, the benefit probably exceeds risk. However, I would like to show that in COVID-recovered 5-11 yos (of which data is sparse), the frequencies and magnitude of vaccine benefit could overlap that of vaccine adverse effects — well below the overwhelming safety margin we should expect for mandated vaccinations of our youth. Keep in mind that while the complications of infection itself may outweigh the adverse effects of vaccination, the former must be multiplied by the risk of infection (or rarer reinfection in the COVID-recovered), to practically compare with the risk of adverse effects (AE) with vaccination.
Currently, there is only limited safety data on 5-11 yos (virtrually none in the COVID-recovered of this age-group). There is some more data in the 12-15yo age range, as published in this NEJM study which is a subgroup analysis of the “pivotal” Pfizer randomized controlled study used for the original adult EUA . While this study concludes in its abstract “there were no vaccine-related serious adverse events and few overall severe adverse events”, a supplementary table from the publication is provided below. (N.B. The Pfizer FDA EUA application released today studies only 2250 participants, with roughly similar results, of which roughly ~1500 got vaccinated. These studies are simply not large enough to detect signal in the <100/100k participant range)
(N.B. “severe” AEs are local or systemic effects that are short of life-threatening, “serious” AEs are death or life-threatening requiring hospitalization, as defined in the study appendix, pg.282).
While questionable in its statistical significance, all AEs were in the range of 5%. There were more overall related adverse effects in the vaccination compared to placebo (2.9% vs. 1.9%) arms. This difference would equate to 1,000/100k (1%) related adverse events. Looking at “severe” adverse events, there was a difference of 0.4% (0.6% vs 0.2%), which equates to 400/100k (0.4%) severe adverse events in the vaccinated, and “serious” adverse effects were less common, but not zero. In the main Pfizer trial 6-month update (for all ages >16yo) published in the NEJM, the vaccination-placebo differences in severe and serious AEs was about 0.5% and 0.1%, respectively. Though these differences can be statistically challenged, short of any further data, let us assume they are real. We can reasonably (and simplistically) estimate that most children will experience mild/moderate AEs in the centered around 1% (100/100k, less common severe AEs in the range of 0.1% (10/100k), and serious/life-threatening AEs at around <0.01% (1/100k).
Other studies confirm these ranges, particularly those of “severe” and “serious” AEs. In this NEJM study focusing on myocarditis only, found a ~2/100k risk of myocarditis in all age groups, but a 10.3/100k risk in males 16-29. And, this extremely elegant study (also published in NEJM) considered the general Israeli population (all ages >16yo, excluding HCWs and COVID-recovered persons), and determined risk differences for a variety of vaccination complications in the range of 2-180/100k vaccinated.
Critics will state that the occurence of vaccine AEs should not be presented alone, and should be compared to comparable complications of SARS-CoV-2 infection — which, I think is a fair critique. After all, the last cited NEJM study (of adults >16yo) did show that complications arising from the infection itself far exceed that of vaccination. However, for our analysis, at least <three> countering points should be made. First, for young children, complications from SARS-CoV-2 infection are likely less prominent - as shown the above CDC data demonstrating extremely low hospitalization and mortality rates in the unvaccinated 5-11yo age group, relative to other age groups. Second, the risk of infection sequalae must be multiplied by the much lower risk of a COVID-recovered reinfection, to arrive at the “absolute” risk, that compares with frequencies of vaccine AEs. Finally, there may be some evidence (although not consensus, and mostly in pre-print literature) that suggests that children and COVID-recovered persons experience more severe vaccine AEs. Nonetheless, it is a fair and conservative assumption that “serious” vaccination AEs lay in the range of 1-10/100k vaccinated.
** Does estimated BENEFIT <exceed or overlap> the RISK of vaccination AEs ? **
Putting this all together, we can now see how the estimated benefits of vaccination in 5-11yos (COVID-naive and COVID-recovered) compare to the the various reported ranges of adverse effects. In this conceptual depiction below, constructed from the assumptions above, the diamonds represent the estimated ranges of infection, hospitalization, and mortality prevented from vaccination, and the gray zones represent the ranges of AEs reported in the above safety/AE articles.
For COVID-recovered 5-11yos, the range of mostly mild-moderate infections prevented are on the order of the mild to moderate side effects experienced. However, for all 5-11yos (COVID-recovered or not), the range of hospitalizations and death sit well in the range of severe and serious adverse effects reported. And, this overlap is especially exaggerated or the COVID-recovered. Bottom line, there is certainly no <overwhelming> benefit to vaccination in COVID-recovered children, over the risk of safety and adverse events.
Note, that these estimates were constructed from near peak baselines 175 cases/week), with conservative assumptions of modest natural immunity protection (75%) and overestimates of COVID-recovered vaccine efficacy (50%) — so, these estimated prevented case ranges could be even lower. We also conservatively assumed that the COVID-recovered experience vaccine AEs at the same rate experienced by the COVID-naive. Therefore, in order to challenge this conclusion, one would have to change these assumptions by orders of magnitude to reach an “overwhelming” threshold worthy of a mandate.
We also must consider that children ages 5-11 y.o. are not simply “little people” with physiology identical to their adult counterparts. The medical field is replete with instances of medications and interventions that are “safe” for adults, but less for children — excessive radiation for example. Children in this age group have developing bodies unique to this pre-pubertal phase, and so we have to consider that the safety data in other age groups may not be exactly transferrable.
Additionally, though admittedly “taboo”, we have to at least consider that these novel mRNA vaccinations, may have longer term and unanticipated chronic effects, beyond what the pivotal and real-world trials can measure — currently limited to less than a year. Absence of evidence is not evidence of absence. The medical record is replete with instances of delayed and critical realizations after confident approvals— like thalidomide, which was originally approved for use in 1952, never tested in pregnant women, and taken off the market in 1961, due to its association with fetal limb malformations. Or, the case of the “superdrug” Vioxx, FDA approved in 1999, but voluntarily taken off the market in 2004 due to safety concerns and heart attacks. The unknown risks that could be determined in the future needs to be tangibly considered today. And, due to their youth, this developing 5-11 yo age group is the most vulnerable to the unknown risks realized in the future
Simply put, the anticipated number of serious illness prevented by the vaccination in COVID-recovered children does not overwhelmingly exceed the known frequency of severe or serious adverse effects and the unknown frequency possible (if even improbable) complications realized in the future.
Final Thoughts
I write this article not as a physician or a clinical data expert — but really as a concerned parent, with an instinctive duty to protect our children by constructively challenging the evidence. I respect objective criticism, and would appreciate any corrections or feedback to the above analysis. I have challenged my own assumptions and played with the various inputs to this model, but cannot realistically get to a point where the prevented infection morbidity comfortably exceeds the threat of severe or serious adverse effects, in the healthy, COVID-recovered child.
I am not the only one to conclude that for healthy children ages 5-11 yo, the absolute benefits of this vaccination overlap the ranges of risk for severe vaccine adversity. The UK Joint Commission on Vaccination and Immunisation essentially conclude exactly the same thing in 12-15 yos:
It is true that the vast majority of children that do get vaccinated will likely experience neither benefit nor harm. This is simply math — as only 1k/100k infections are prevented in the vaccinated COVID-recovered child, 99% would not experience any benefit, and 99% will not experience a severe adverse effect. And so, to that end, I do support the parental option of vaccinating their young (even if COVID-recovered) children, if they so choose. Children with multiple comorbidities, for example, may benefit from the vaccination. However, on moral grounds, you cannot mandate an intervention in a healthy or recovered child, in which the benefit does not overwhelmingly exceed risk — and this is especially true in the healthy COVID-recovered child.
Proponents of vaccination mandates in children will undoubtedly point towards a number of intuitive arguments to justify their position. One argument is the precedent of other vaccination requirements in place (MMR, Polio, TDap, etc.) — while those vaccinations have now been around for decades, the Pfizer mRNA vaccination is the first of its type, with no long-term safety data. Sorry, the experts’ overconfidence on safety is not a substitute for careful safety trials. This should be demanded. Another argument is the “public benefit” realized by mass vaccination. This is individual vs. collective dispute is for politicians — but as scientists, we have no evidence that the COVID-recovered present any greater transmission risk than their vaccinated counterparts. In fact, this rare study on transmission suggests at least equivalency.
So, rather than enforce heavy-handed mandates on our most vulnerable and innocent citizens, our public health leaders must begin to embrace policy nuance. Let us start by recognizing that children 5-11yo need individual assessment, based on their prior infection status, serological status, pre-existing comorbidities, and other risk factors. Make the vaccine optional for those parents who deem it necessary for the protection of their at-risk child. But, to the FDA and CDC: please at least acknowledge that in certain segments of this age group, a rigid mandate puts healthy and COVID-recovered children in harm’s way.
If you got down to here, thank you for reading.
(DISCLAIMER: This article represents my opinion only, and not of any organization I am affiliated with. It based upon best efforts to compile and analyze the data and evidence. The intended use is for policy discussion purposes only. It is not a substitute for advice from a personal physician. Please consult your personal physician for health advice.)










Hello Dr. Shenai, thank you for this detailed analysis. This is pretty much exactly how I feel and I am not going to be signing up my kids for any early waves of this vaccine. That being said, how should I respond to someone who posits that myocarditis rates are greater via natural COVID infection? Should I counter-respond by asking that these myocarditis rates be broken down by age, gender and prevalence of comorbidities in those affected kids? (As my kids are young, fully healthy, thin and not obese)
Consulting your personal physician could be the worst thing you can do - they do not take the time to do any research and only parrot the dictates of the public health authorities, which are deeply corrupt.